
On Halloween, I attended the Reimagine: End of Life workshop called Graphic Medicine, Reflective Drawing, and Advanced Care Directives at the 53rd Street library. It was led by MK Czerwiec, author of Taking Turns: Stories from HIV/AIDS Care Unit 371. MK is one of the founders of Graphic Medicine, a genre of patient and caregiver narratives in a comics format.
As soon MK began to unpack her supplies, putting a brand new (!) pack of 24 Crayola crayons at each chair, I knew I was in the right place: we were going to draw! My giddiness was echoed in the voices of the other participants. Most of us were middle aged or older, but the moment we opened our boxes and inhaled that signature crayon smell, we were immediately nostalgic. I was transported (way) back to elementary school—that glorious time when I was allowed to call myself an artist.
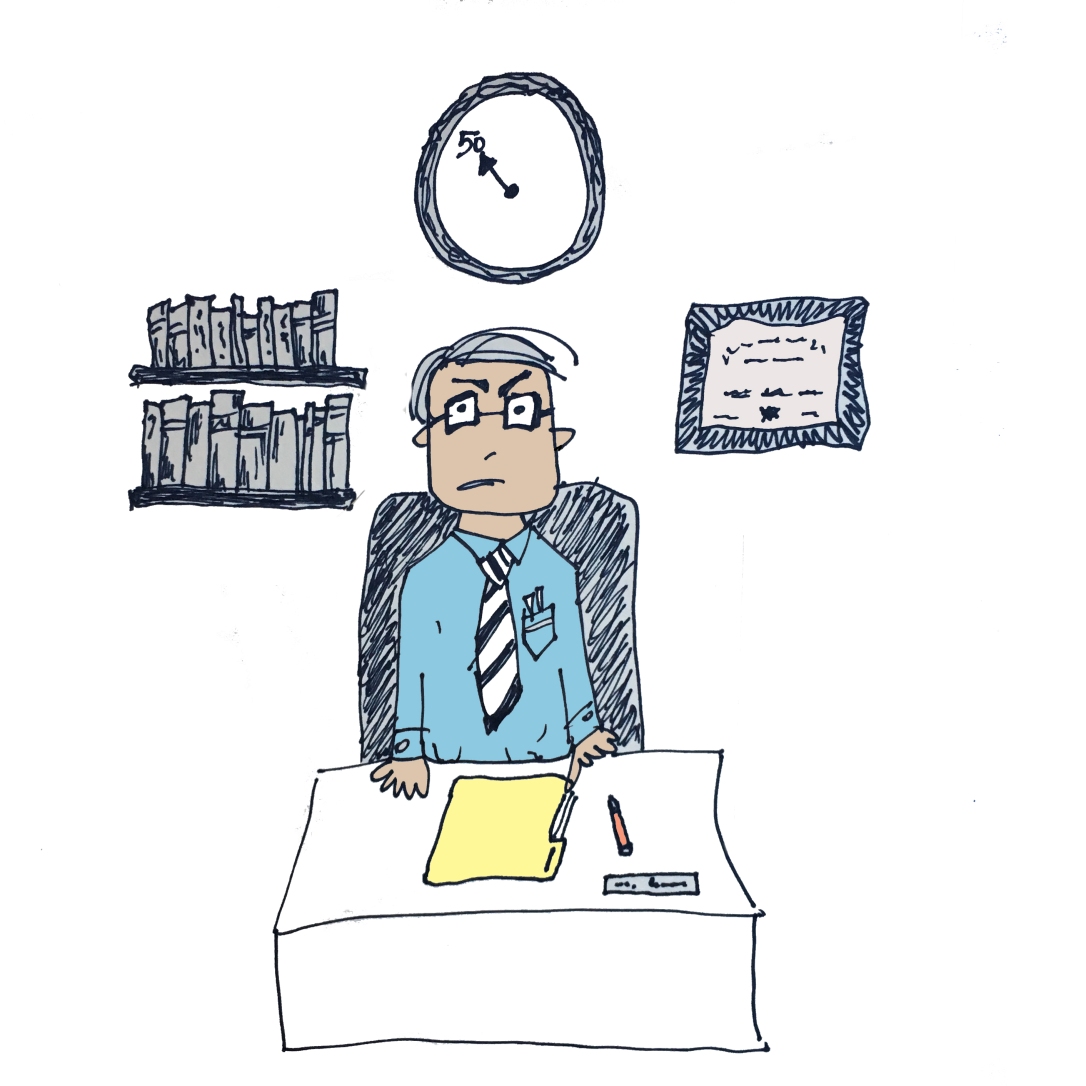
Our first task was fairly simple: draw a self-portrait in “portrait mode.” I began immediately, drawing my typical doodle: huge hair, hands on hips, not-smiley, almost defiant “hmph” face, big glasses. I heard my professor comment from across the table, “No fair. Jen has practice doing this.”

We shared our drawings as a way to introduce ourselves, and gave our reasons for attending this workshop. Some of us were getting older and wanted a way to start thinking about their end-of-life decisions, a few were healthcare practitioners, and others were children of aging parents. More than one of us identified as “Graphic Medicine groupies.” One gentleman said he wanted to be more “easy with himself and others” as he aged. Another participant was a self-described “aspiring minimalist,” who was hoping to pare down belongings as she aged.
Most adults do not draw on a regular basis. MK asked us to speculate why this is. We spoke for a moment about the power of crayons: they remind us of a time when we were less inhibited, when we were encouraged to be creative with little expectation or judgment. No matter how old we may be, we can all stand to benefit from “kid thinking.”
Our next assignment was to hold the paper “landscape style” and draw a good death. We had seven minutes. People got to work immediately, and when it was time to share, many of us were still adding finishing touches. One drawing depicted a series of faces in rainbow shades connected by a line indicating our shared humanity and the cycle of life. Others featured scenes involving nature and blue skies and family and friends. One woman shared her process: her first priority was eating as much chocolate as possible, and only when this was in place did she add lower-priority elements like family and friends (you gotta love that honesty). My drawing was a series of faces in black crayon with speech bubbles. The voices were saying things like, “You can go now. I love you.”
As we were sharing, MK asked us about particular decisions that we made in our work. She spoke to us as if we were legitimate artists sharing our work in a gallery, with comments like “You’re the artist. You make all the choices” and “You are in charge of what this means.” Many of us felt like these alleged decisions were more a function of our limitations rather than our aesthetic acumen. MK offered us a challenge to nourish our artistic selves: draw a self-portrait each day.
So what does one drawing about the end of life have to do with advanced directives? An illustration like this could be a starting point for a conversation about our end-of-life priorities, and MK offered some extensions of this. One was to make our “good death” drawing the center panel of a three-panel comic. What comes before? What comes after? Another prompt would be to draw (then describe) the ideal decision-maker, listing the qualities that would make someone a good healthcare proxy.
It was really incredible to see that a bunch of strangers, each with a box of crayons, could connect so deeply in such a brief period of time. I hate to admit it, but this only child might not have been so nice if she had been forced to share.
Hmph.

 So, who prescribed your medicines in 1994?
So, who prescribed your medicines in 1994?